 Researchers do not know exactly what causes Sudden Infant Death Syndrome (SIDS). However, they do have an informed idea, or theory, that may explain how SIDS happens.
Researchers do not know exactly what causes Sudden Infant Death Syndrome (SIDS). However, they do have an informed idea, or theory, that may explain how SIDS happens.
Searching for Clues
Researchers have found problems in the brains of babies who died from SIDS. In some cases, the problem was found in a network of nerve cells in a part of the brain that controls breathing, heart rate, blood pressure, temperature, and waking from sleep. Other research suggests that changes in the baby’s genes may cause problems with how the body functions, including breathing and waking from sleep.1
Researchers also found that babies who died from SIDS had high levels of serotonin in their blood.2 This finding could suggest a problem with how the body uses serotonin, a chemical that carries messages between nerves. Out-of-balance levels of serotonin could affect how the baby’s body handles regular functions or everyday processes, like waking from sleep and breathing.
There is currently no way to detect these problems when a baby is alive. Scientists also believe that these issues alone may not be enough to cause death.
A Framework for Understanding How SIDS May Occur
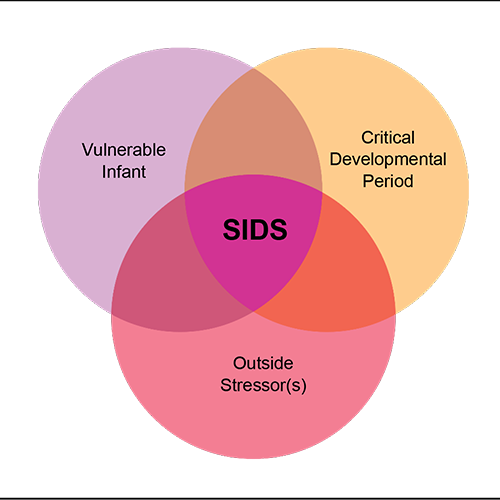
Researchers use the Triple-Risk Model to describe how a SIDS death may happen.
- First, the baby has one or more unknown medical conditions, such as a brain or genetic problem that affects the heart rate or breathing. There is no way for healthcare providers or parents to know about these medical conditions.
- Then the baby goes through an important period of development. In their first 6 months, babies go through periods of fast growth and changes, such as changes in blood pressure, breathing, and sleeping patterns. During these periods, their body may be unstable and react in unusual or unexpected ways.
- Lastly, the baby encounters one or more outside stressors, such as being placed on their stomach to sleep or being exposed to secondhand smoke in their environment. These things put additional stress on the body or how it functions.

By itself, each risk situation is usually not a problem. Most babies can adjust to stresses and changes in body system function and recover from these factors if they occur alone or even two at a time. However, when all three occur at the same time, a death from SIDS becomes more likely.
For example, a baby with an unknown and undetectable medical condition starts going through a normal developmental period that makes the breathing system unstable. If an outside stressor, like being placed on the stomach to sleep, occurs at the same time, the baby may not be able to overcome all three factors to continue breathing normally. The baby may die, and the cause of death may be SIDS.
Because outside stressors are the only factor in the Triple-Risk Model that caregivers can control or change, the Safe to Sleep® campaign focuses on reducing or eliminating outside stressors.

